by Tiffany Coppock, AIA, NCARB, CDT, ASTM, RCI, EDAC, LEED AP, and Angela Ogino
When specifying insulation systems for healthcare facilities, architects and contractors can borrow wisdom from the world of real estate: it is all about location, location, location. Specifying the right type of insulation to address the performance challenges in various locations within the healthcare facility enclosure can not only support the building’s performance objectives, but also help meet life-safety, comfort, and sustainability goals.
It is important to look beyond the frequently discussed thermal properties of insulation to consider how it addresses life-safety, moisture management, privacy, and sustainability challenges in healthcare enclosures. Before addressing the use of insulation in specific areas of the healthcare enclosure, it is helpful to take a broader look at construction and healthcare trends.
Connecting evidence-based design to patient outcomes
The United States still continues to see high rates of new construction and remodeling in the healthcare environment. According to Joint Commission International’s 2017 report, “Planning, Design, and Construction of Healthcare Facilities,” increases in healthcare facility spending are driven in part by an aging population that is living longer (see “Planning, Design, and Construction of Healthcare Facilities,” from Joint Commission Resources). The growing need for safe, efficient care environments is spurring both new construction and medical facility remodeling in the country.
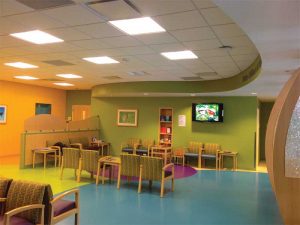
As healthcare construction activity increases, evidence-based design is influencing decisions throughout the architecture, engineering, and construction (AEC) community. As the name implies, this process involves making decisions about the built environment based on credible research to achieve the best possible results. According to the Joint Commission, it may lead to positive patient outcomes such as shorter hospital stays and improved morale due to environmental design factors (e.g. more natural light in patient rooms) or result in fewer medication errors because well-lit and isolated medication prep rooms encourage focus.
These findings are supported by a breadth of other research reports. In fact, more than 600 studies have linked the built environment to factors such as patient satisfaction, stress, health outcomes, and overall quality of care (for more information, consult “Healing environment: A review of the impact of physical environmental factors on users,” published in Building and Environment in December 2012). Conversations with directors overseeing these facilities provide further anecdotal evidence the healthcare environment affects patients’ satisfaction.
Different areas of the healthcare facility present distinct challenges when it comes to the insulation material specified. Whether insulation is used in a vegetated roof assembly atop a hospital to provide a positive view of nature while managing moisture, in walls and ceilings to improve acoustic performance, or to support passive life-safety systems, this element is integral to achieving performance goals.
Start with size, function, and occupants

Whether a research and teaching hospital or a rehabilitation center, specifying insulation in the healthcare facility begins with a thorough understanding of the building’s size and function, as well as the occupants it serves. A building’s occupancy classification, along with the number of floors and square footage, will determine the building code requirements and subsequently influence the materials specified for the enclosure.
The International Building Code (IBC) includes dozens of different occupational classifications covering everything from assisted living facilities and medical spas to drug rehab centers, ambulatory surgery facilities, and research hospitals. Hospitals are classified as Institutional Group 1 or 2 occupancy, while ambulatory clinics (facilities with less than a 24-hour patient stay) are often classified as Business Group occupancy. Institutional Group 1 occupancy includes those capable of slow evacuation, while Institutional Group 2 includes those incapable of self-preservation.
Occupancy classifications such as institutional and business identify the capability of occupants of self-preservation in relation to risks. In turn, specific construction types and height and area requirements are imposed based on different occupancy types. For example, Institutional I-2 category buildings have special requirements listed in Section 407, “Group I-2,” of IBC, including those related to corridor construction, exit distances, limits to sleeping areas, and essential electrical supply.
Many facilities will include both institutional and business occupancies—for example, administrative and outpatient offices located in a building that houses surgical suites.
When more than one occupancy is permitted, compartmentation may be allowed by demising walls of specific fire and smoke resistance. Various standards present additional requirements for hospitals, such as fire and smoke protection, egress, and isolation. Some of these standards include those set by the Joint Commission, College of American Pathologists (CAP), Facility Guidelines Institute (FGI), Medicaid, and Medicare, as well as the Occupational Safety and Health Administration (OSHA), along with Hospital Consumer Assessment of Healthcare Providers and Systems (HCAPS) scores. While codes set the baseline standard for compliance, achieving performance objectives requires consideration of each area within the enclosure.
The nature of the occupants served also drives decisions regarding safety systems in the healthcare facility. Are the occupants very old, very young, sedated, or connected to equipment? Are oxygen and other flammable materials in proximity to the patients? As life safety is such an integral issue, it is best to start by examining the perimeter of the healthcare enclosure and the special considerations that come into play when specifying insulation for the perimeter fire containment system.
Life safety and perimeter fire containment
Passive fire containment—also referred to as compartmentation—complements and enhances a building’s active and detective life-safety systems. Unlike active systems (e.g. sprinklers) and detection systems (e.g. smoke and heat detectors), passive systems operate without external activation once correctly installed. As such, they are an integral part of a comprehensive approach to fire containment.