The New Era of Healthcare Acoustics: Specifying optimal ceiling performance for hospitals

by Gary Madaras, PhD, Assoc. AIA
Designers and specifiers need to react quickly to increasing demands by healthcare executives, caregivers, and patients for better acoustic quality in their facilities.
High noise levels in hospitals have been shown to adversely affect patient and staff physiological conditions, including heart rate, blood pressure, respiration rate, skin conductance, and muscle tension.1 Noise decreases the duration and quality of the patient’s natural sleep cycles and inhibits recovery. Conversely, when the areas around patient rooms are quiet, occupants sleep better.
Restorative sleep decreases the need for pain medication, reduces patient fall rates, lowers average length of stays, and improves medical outcomes. In this new era of healthcare, acoustic performance is a top priority, not only in existing facilities, but also in every renovation, expansion, and replacement facility currently on the drawing board.
There are no other architectural surfaces more important and available to reduce noise and promote accurate speech communication in healthcare facilities than the ceilings. Considered to be no/low-contact ‘housekeeping surfaces’ by the Centers for Disease Control and Prevention (CDC), they do not significantly contribute to nosocomial infections rates. This allows a facility’s ceilings, in most areas, to be acoustically treated for either noise control or accurate speech communication.
In a 2007 Center for Health Design (CHD) whitepaper, “Sound Control for Improved Outcomes in Healthcare Settings,” the authors concluded installing high-performance acoustic ceiling panel systems is a key environmental strategy to reduce noise (and associated perceptions), as well as to have a positive impact on outcomes such as improved speech intelligibility and reduced perceived work pressure among staff.2
Changing demographics, changing healthcare design
Earlier this year, a biannual benchmarking study conducted by the Beryl Institute showed more than 70 percent of healthcare professionals cited patient satisfaction as one of their top priorities during the next three years.3 Further, they said noise reduction was their top priority for improving patient satisfaction. To understand these findings, one must understand the series of events that has unfolded in the United States over the last eight years.
As baby boomers enter the phase of their lives where greater healthcare is likely to be required, and as obesity-related medical problems continue to increase, a deficit between Medicare revenues and spending was projected. In response, the 2005 Deficit Reduction Act authorized the Centers for Medicare and Medicaid Services (CMS) to implement its value-based purchasing (VBP) program. This program withholds one percent (incrementally increasing to two percent by 2017) of hospital financial reimbursements for care of Medicare patients. Those hospitals with higher quality and performance receive not only the one percent originally withheld, but also up to an additional one percent withheld from lower performing hospitals.
Currently, 30 percent of a hospital’s VBP score comes from the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey given to inpatients.4 This survey assesses their satisfaction with aspects of care such as doctor and nurse communication, pain management, and room cleanliness. At first, hospitals received full reimbursement for implementing the survey and reporting the results, regardless of the actual scores. But as of October 2012, actual reimbursements to hospitals are getting adjusted up or down, in part due to the facility’s acoustics.
In the HCAHPS survey, the question, “How often was the area around your room quiet at night: always, usually, sometimes, or never?” consistently scored the lowest. The current national top-box (i.e. “always”) score is only 60 percent compared to an average of 73 percent for all other metrics. Discharge Information has a top-box score of 84 percent. A high score on the quiet-at-night question is not easily achieved in existing hospitals.
A 2012 study conducted by Making Hospitals Quiet and the Beryl Institute showed only 12 percent of 241 hospitals trying to reduce noise in existing facilities judged their progress as “good” or “great.”5 A high score is not easy to achieve in new hospitals either. Twenty-five new (ground-up) hospitals built in the last six years have an average quiet-at-night score of 62 percent—only two percent better than the U.S. average.
The VBP program does not allow for even one low HCAHPS outlier. Many hospitals are seeing their reimbursement rates held down by their quiet-at-night score even though scores for the other metrics might be above achievement thresholds. There is also a strong indirect relationship between the quiet-at-night score and the scores of other questions. For example, when quiet-at-night scores increase, so do the scores for doctor communication, nurse communication, and even pain management.

Entering evidence-based design
Evidence-based design (EBD) is the process of basing decisions about the built environment on credible research to achieve the best possible outcomes. A growing body of evidence attests to the fact the physical environment influences safety, patient stress, staff effectiveness, and quality of care provided in healthcare settings. At least three EBD studies have shown installing high-performance acoustic ceiling panel systems reduce noise propagation, creates the perception of a quieter environment, and improves speech intelligibility to enhance accuracy of staff communications.
In addition to the EBD studies involving high-performance acoustic ceiling panel systems, a 2008 whitepaper by the Center for Health Design and the Georgia Institute of Technology—“The Business Case for Building Better Hospitals through Evidence-based Design”—specified a list of eight “priority design recommendations” based on the strength of the evidence available and the impact on safety, quality, and cost. One of these priority design recommendations is to install high-performance acoustic ceiling panel systems to decrease patient and staff stress, reduce patient sleep deprivation, and increase patient satisfaction.
The whitepaper’s authors concluded:
Hospital leaders and boards face a new reality: They can no longer tolerate allowing preventable patient hospital-acquired conditions such as infections and falls, injuries to staff, unnecessary intra-hospital patient transfers that can increase errors, or have patients and families subjected to noisy, confusing environments that increase anxiety and stress. They must effectively deploy all reasonable quality-improvement techniques available.
To be optimally effective, techniques will almost always harness a bundle of tactics that, when implemented in an integrated way, will produce best results. Leaders must understand the clear connection between constructing well designed healing environments and improved healthcare safety and quality for patients, families, and staff, as well as the compelling business case for doing so. The physical environment in which people work and patients receive their care is one of the essential elements to address a number of preventable hospital-acquired conditions.
Roadmap to minimum acoustic requirements
The first step in understanding high-performance acoustic ceiling panel systems and how to specify them is to understand the standards and guidelines that establish minimally acceptable acoustic performance. From there, one can better understand best practices.
When trying to comply with the acoustic requirements in the different standards and guidelines for healthcare facilities, it helps to understand which document is the core source for acoustic performance criteria and design recommendations, and which other documents draw their content, in part or whole, from that core document.
Acoustics Research Council (ARC) represents several hundred members of the leading acoustical societies in the United States, including those from the Acoustical Society of America (ASA), the Institute of Noise Control Engineers (INCE-USA), and the National Council of Acoustical Consultants (NCAC). Since 2005, ARC has been responsible for developing the core document on acoustical performance criteria in healthcare facilities. The current version is the 2010 Sound & Vibration Design Guidelines for Health Care Facilities (v2.0), which is on a four-year revision cycle with the next version due out in early 2014.6 This core document is a minimum design requirement to ensure satisfactory acoustics and privacy in healthcare facilities of all types.
The main organization that references parts of this core acoustics document is the Facility Guidelines Institute (FGI). Founded in 1998 to provide continuity in the revision process of what were originally minimum construction standards from the Department of Health and Human Services (DHHS), FGI has produced the Guidelines for Design and Construction of Health Care Facilities—the 2010 edition is now used in some form by 42 states.7
The FGI Acoustics Working Group has become synonymous with ARC. Its efforts resulted in the 2010 version of FGI’s guidelines—the first edition in its 60-year history to contain comprehensive minimum criteria for acoustics in healthcare facilities. It recently revised the acoustics criteria in the 2010 version for the next issuing of FGI guidelines.
Revisions to FGI’s guidelines also occur on a four-year cycle. The 2010 version recently has been through a complete revision cycle, and the next version will be released early in 2014. In previous editions, only one guideline covered all types of healthcare facilities. In 2014, this will be split into two separate guidelines:
- Guidelines for the Design and Construction of Hospitals and Outpatient Facilities, which will cover hospitals and outpatient facilities; and
- Guidelines for Design and Construction of Residential, Health, Care, and Support Facilities, which will cover residential healthcare facilities such as assisted living, hospices, and nursing homes, along with related support facilities such as wellness centers, adult daycare facilities, and outpatient rehabilitation therapy facilities.
Some of the content in this new guideline existed in the previous versions, but it will be split off, expanded, and made to stand on its own in 2014.

The FGI Acoustics Working Group cautions that the rapid pace of change in the U.S. healthcare industry (and in standards organizations) means each subsequent edition of the FGI’s guidelines likely will contain additions and revisions to the acoustical criteria to meet the healthcare industry’s growing need for guidance about sound, privacy, and noise.
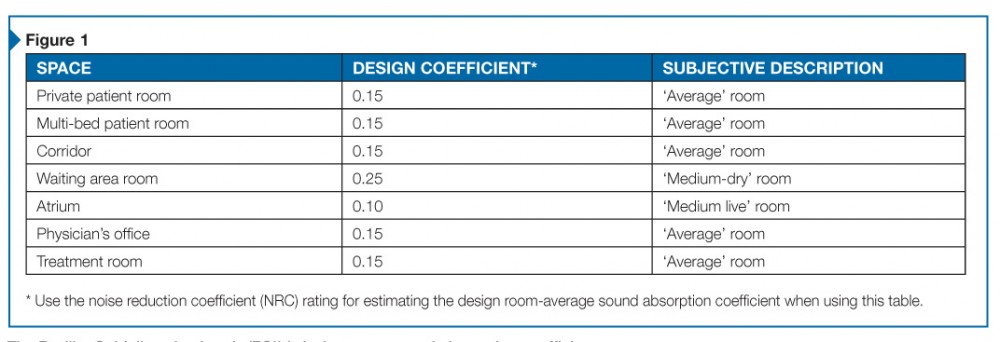
In FGI’s 2010 guidelines, Section 1.2-6.1.3, “Design Criteria for Acoustic Finishes,” requires all normally occupied healthcare facility spaces to incorporate acoustic finishes to achieve the requirements as indicated in Table 1.2-1, “Design Room Sound Absorption Coefficients.” This numeric value is an average sound absorption coefficient for all room surfaces weighted by their relative areas (Figure 1).
In this table, with the exception of a few room types, the minimum required design room sound absorption coefficient is 0.15, which subjectively characterizes the room as ‘average.’ Although all room types are not listed in Table 1.2-1, there is still the overarching statement in section 1.2-6.1.3 that “all normally occupied spaces shall incorporate acoustic finishes.”
If one assumes the floor material is sound-reflective (e.g. terrazzo, vinyl composition tile [VCT], or laminate) and assumes the wall materials are also sound-reflective (e.g. painted gypsum board, glass, laminate, or finished wood), then meeting the required design room sound absorption coefficient of 0.15 falls mostly on the ceiling material.
The most popular acoustic ceiling panel systems are composed of mineral fibers, fiberglass, inorganic perlite blends, or perforated metal panels with an acoustical blanket. These panels are usually installed in a metal suspension grid to create the ceiling system. Meeting the 0.15 minimum requirement with these ceiling materials is not that difficult, many spaces can achieve this with minimum performing acoustic ceiling panel systems available from most ceiling manufacturers.
In general, specifying a ceiling panel with a noise reduction coefficient (NRC) of 0.50 will meet the 0.15 design room sound absorption coefficient in the FGI guidelines. A qualified acoustics consultant should calculate the actual design room sound absorption coefficients for the project to ensure requirements are being met.
At the 21st International Congress on Acoustics (ICA) in Montréal in June 2013, the Acoustics Working Group that edited the 2010 FGI guidelines into the 2014 version reported the minimum design room sound absorption coefficients may be increasing from 0.15 to 0.20, in FGI’s new Guidelines for Residential, Health, Care, and Support Facilities. At the time of the presentation, it was not clear whether the same change would be made in the Guidelines for Hospitals and Outpatient Facilities or if the value would remain at 0.15. This increase means that in most cases, minimal performing acoustic ceiling panels (i.e. NRC 0.50) will no longer meet the requirements in the FGI guidelines. Instead, as a general rule, moderate performing ceiling panels with an NRC of 0.70 will be required.
The Joint Commission (JC) is the not-for-profit organization that accredits and certifies more than 20,000 healthcare organizations and programs in the United States. The JC does not mandate use of FGI’s guidelines if another state or national standard is being applied to the project. For example, the Veterans Administration (VA) and Department of Defense (DOD) have developed their own guidelines. Beginning in January 2011, JC simply references the 2010 edition of FGI’s guidelines in its accreditation manuals.
CMS does not demand compliance with FGI’s guidelines either, but it does require compliance with an established standard and local building codes and requirements. Therefore, since many states call for compliance with the FGI guidelines, it makes them a back-door requirement for the JC and CMS in those jurisdictions.
The acoustic requirements in the 2010 version of FGI’s guidelines and its reference document, Sound and Vibration Design Guidelines for Health Care Facilities, are the basis for the acoustic requirements in the current version of the U.S. Green Building Council’s (USGBC’s) Leadership in Energy and Environmental Design (LEED) for Healthcare program (v.2009), as well as the upcoming edition (v4, currently in beta testing). Two LEED points are available for acoustic performance in Indoor Environmental Quality (EQ) Credit 2, Acoustic Environment.
Similarly, the acoustic requirements in the latest version of the Green Guide for Health Care GGHC (v2.2, 2007) are adopted from the 2006 version of the Sound & Vibration Design Guidelines for Health Care Facilities. It previously was titled the American Institute of Architects’ (AIA’s) and American Hospital Association’s (AHA’s) “Draft Interim Sound and Vibration Design Guidelines for Hospital and Healthcare Facilities.” GGHG, like LEED, has two points available for proper design of the acoustic environment (EQ 9.1 and EQ 9.2).

Specifying high-performance acoustic ceiling systems
Early in the design process of every healthcare building, designers, specifiers, and healthcare executives must make an important decision: “Are we designing a minimally acceptable facility, or an optimal environment for generative recovery, healing, and health?” The answer to this question determines what type of ceiling will be specified and possibly need to be defended as the design, documentation, and construction take shape.
When specifying high-performance acoustic ceiling systems, there are three main acoustic metrics: the aforementioned NRC, along with articulation class (AC) and ceiling attenuation class (CAC). NRC and AC both indicate the ceiling’s ability to absorb sound inside a space and are fairly well correlated—generally, if NRC increases, so does AC. The main difference is the former is a better indicator of a ceiling’s (or other surface’s) ability to reduce general reverberation of noise as it reflects around inside spaces or down corridors throughout time. AC is a better indicator of how much a single reflection off the ceiling is attenuated.
If the general concern is overall noise and reverberation reduction, then the correct metric to specify is NRC. Values range from 0.0 (i.e. highly reflective) to more than 1.0 (i.e. very absorptive). NRC values of 0.60 or less are considered ‘low,’ from 0.65 to 0.85, ‘moderate,’ and above 0.90, ‘high.’ In rooms or areas such as inpatient corridors, centralized nurses’ stations, waiting areas, private patient rooms, and quiet rooms, reducing noise and reverberation are the primary concern. For these spaces, optimal performance equates to specification of very high NRC values in the range of 0.90 to over 1.0.
If the general concern is privacy and confidentiality between areas in close proximity that are not separated by enclosed isolating construction, then the correct metric to specify is AC. Values range from around 120 (i.e. high reflectivity, low confidentiality) to more than 230 (i.e. high attenuation, high confidentiality). AC values of 160 or less are considered ‘low,’ from 170 to 180, ‘moderate,’ and 190 and above, ‘high.’ In spaces where auditory privacy is a concern (e.g. semi-private patient rooms, pre- or post-operative communal areas, registration, financial services, and open consultation areas), optimal performance equates to very high AC values in the range of 190 to 230.
The next type of metric, CAC, is not a measure of noise absorption/attenuation, but instead a measure of the ceiling’s ability to block transmission of noise from the plenum above the ceiling down into the space below the ceiling. If there is no significant noise in the plenum above the ceiling, then CAC is not a metric of concern. However, when evaluating potential noise in the plenum, one must consider:
- noise (or private conversations) that might flank over demising walls that do not extend all the way up to the underside of the slab above;
- impact noise on the slab/roof above; and
- noise that can break out of ductwork located close to the fans in the air-handling units (AHUs).
One of the biggest mistakes specifiers can make is to just select a moderate CAC value for the ceiling instead of taking the time to consider whether CAC is relevant. More often, CAC is not important. Since moderate to high CAC panels typically have significantly lower sound absorption qualities (i.e. NRC and AC), specifiers may be sacrificing acoustic comfort, privacy, confidentiality, and intelligibility for isolation from noise that does not exist in the plenum.
CAC values range from 0 (i.e. no ability to block transmission) to more than 40 (i.e. high ability to block transmission). CAC values of 25 or less are considered ‘low,’ from 25 to 35, ‘moderate,’ and above 35, ‘high.’ A good example of where CAC is important is an older medical office building where demising walls between treatment rooms stop just above the ceiling and the plenum above the ceiling provides a path by which private conversations easily pass between rooms. In cases such as this, CAC values for the ceiling should be 35 or higher.
It should be understood all these acoustic metrics—NRC, AC, and CAC—are single-number indicators, and are intended to represent the ceiling’s performance across a wide band of frequencies. However, the three metrics have been calculated from a more useful and telling data set indicating the ceiling’s actual performance at individual 1/3-octave bands (i.e. many narrower groups of frequencies). While it is acceptable to specify NRC, AC, and CAC, the specifications for high-performance acoustic ceilings should also include the minimum performance requirements at individual frequency groupings (i.e. 1/3 octave bands).
Manufacturers must have these data in order to report NRC, AC, and CAC values. For example, in the medical office building where the demising walls stop at the ceiling and a common plenum provides a path for private conversations to be heard in adjacent rooms, the optimal ceiling specification would not be a single CAC value. Different ceilings with the same CAC value can perform significantly different in their ability to mute private conversations. Less critical is the CAC value. Most important is the 1/3-octave band transmission loss values in the 2- and 4-kHz octave bands. These are the most important frequencies for making speech intelligible. Therefore, to ensure private conversations remain private, one should specify the transmission loss (double pass per ASTM E1414, Standard Test Method for Airborne Sound Attenuation Between Rooms Sharing a Common Ceiling Plenum) not be less than 40 dB per 1/3-octave band in the 2- and 4-kHz octave bands.
Beyond absorbing noise for the sake of comfort, privacy, and confidentiality, another acoustic performance goal is accurate, intelligible, speech communication. In meeting or conference rooms, procedure rooms requiring team communication, worship centers, music therapy rooms, group education rooms, and geriatric care areas, the ceiling’s role is not one of absorption, but instead of passive reinforcement of the spoken word. Loud reflections off the ceiling help listeners hear and understand what is being said. It helps them feel closer to, and more intimate with, the people speaking. It helps them to concentrate and remember.
In these cases, ceilings should have low NRC and AC values (i.e. <0.30 and <140 respectively), and maximum, rather than minimum, levels should be specified. Optimally, one must ensure preservation of the most important speech frequencies by specifying absorption coefficients (alphas) shall not exceed 0.30 in any 1/3-octave band in the 2- or 4-kHz octave bands. However, as a precaution, it is important to ensure recommended reverberation times are not exceeded by sizing the room appropriately and, if needed, specifying absorptive materials on the floor and walls.
Acoustic materials and nosocomial infection rates
In early 2012, Chicago’s Rush University Medical Center opened its $654-million expansion, including a new emergency center, a neonatal ICU, and 304 acute patient rooms. During the design process, the nurse researchers were charged with determining whether there was any evidence demonstrating an increase in nosocomial infection rates due to the presence of acoustic materials. Finding none, and recognizing the noise control benefits, they recommended use of acoustic materials in the new hospital. The floors in the patient care areas are carpeted and the ceilings are high-performing acoustic ceiling panel systems.
Despite Rush University conclusions and a growing understanding about the safe and beneficial use of acoustics materials in healthcare facilities, there has been a lingering misconception that the use of acoustic materials in healthcare facilities, particularly hospitals, increases nosocomial infection rates. This misconception exists more so with healthcare providers than with designers of healthcare facilities.
In fact, the available information on the topic supports there is no relationship between the use of acoustic materials and hospital-acquired infection rates. Since 1970, CDC and AHA have advocated discontinuation of routine environmental culturing because rates of healthcare-associated infection have not been correlated with levels of general microbial contamination of environmental surfaces.
In 2003, CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC) published their Guidelines for Environmental Infection Control in Healthcare Facilities.8 These groups scoured the available evidence on the transmission paths for infection and developed guidelines for controlling the spread of infections in healthcare facilities.
Although microbiologically contaminated surfaces can serve as reservoirs of potential pathogens, these surfaces generally are not directly associated with transmission of infections to either staff or patients. The transferal of microorganisms from environmental surfaces to patients is largely via hand contact with the surface. Therefore, CDC’s guidelines discuss the impact of environmental surfaces on infection prevention in terms of the likelihood of hand contact.

CDC categorizes floors, walls, and ceilings as ‘housekeeping surfaces,’ further defining floors and ceilings as minimal hand-contact surfaces. The CDC guidelines include no recommendations against use of carpeting in healthcare facilities, but do suggest avoidance of carpet in areas around sinks such as in laboratories or janitor’s closets where they are likely to get repeatedly wet and in areas for immunosuppressed patients. However, carpeting offers limited noise control efficacy because it is a thin material and, as such, mostly absorbs only high-frequency noise effectively. The real opportunity for noise control and in some locations promotion of accurate speech communication remains to be the ceiling.
Discussion of ceilings in the CDC guidelines is limited. This is likely due to ceilings being no-contact surfaces (except during maintenance procedures). One could reasonably deduce that if there are no increased risks of nosocomial infections due to carpeting on floors then there would not be increased risks due to acoustical ceilings. The CDC’s guidelines encourage that ceilings (like all room surfaces) are well-sealed to help protect against undesired air infiltration, and that these surfaces do not collect an unusual amount of dust. There is no mention of cleaning ceilings beyond a general recommendation to keep all housekeeping surfaces visibly clean on a regular basis.
It should be noted all CDC recommendations on housekeeping surfaces are Category II, meaning “suggested for implementation,” as opposed to Category IA or IB, meaning “strongly recommended,” or Category IC, meaning “required by state or federal regulation.”
New criteria for acoustic success
In the past, the acoustic success of a hospital was largely judged by whether noise was present or not. Noise was bad and quiet was good. Still, silence is not the goal, as it makes high-acuity patients feel isolated. Nurse call rates increase. Further, a sonically sterile environment is a tremendous loss of opportunity. The new era of healthcare acoustics is not just about eliminating bad noises, but also about employing good sounds for their beneficial attributes.
Auditory landmarks are now used to aid wayfinding. The soft sounds of a baby cooing can lead expectant parents toward obstetrics. Positive auditory distractions, especially those that are interactive, can distract patients from their pain and loved ones from their stress. Nature sounds, whether real or recorded, are an important part reaping the benefits of having access to the natural world. Certain types of music can return worsened physiological conditions back to normalcy faster than manmade noise or silence. Acoustic experts currently are working on defining and developing guidelines for these more advanced aspects of enhanced sound quality in healthcare facilities.
In the future, the acoustic success of hospitals will be judged by how the total auditory experience contributes to recovery and satisfaction for patients, accuracy and stress relief in caregivers, and maximization of financial reimbursements.
Notes
1 For example, see the white paper “Noise Pollution in Hospitals: Impact on Patients,” by Timothy Hsu, PhD, et al. Visit www.turner-white.com/pdf/jcom_jul12_noise.pdf. (back to top)
2 The article, by Anjali Joseph (Center for Health Design) and Roger Ulrich (Center for Health Systems and Design, Texas A&M University) can be read at www.healthdesign.org/sites/default/files/Sound%20Control.pdf. (back to top)
3 Visit www.theberylinstitute.org/?page=PXBENCHMARKING. (back to top)
4 Visit www.hcahpsonline.org/home.aspx. (back to top)
5 Visit theberylinstitute.site-ym.com/store/view_product.asp?id=1101753. (back to top)
6 Visit speechprivacy.org/joomla//index.php?option=com_content&task=view&id=33&Itemid=46. (back to top)
7 Some states have adopted the whole document, and a few of those automatically update to the current edition (i.e. 2010) when it was published. Other states only use part of the document, often the “General Hospitals” chapter, to regulate facilities and only use the rest as a reference. Many states reference an earlier edition. Some states also modify language in FGI’s guidelines to address their own specific issues. (Other states write their own code with little input from FGI’s guidelines.) To find out what is most applicable for a project, the designer should contact the pertinent state agency (often the Department of Health) or e-mail info@fgiguidelines.org. (back to top)
8 Visit www.cdc.gov/mmwr/preview/mmwrhtml/rr5210a1.htm. (back to top)
Gary Madaras, PhD, Assoc. AIA, is a healthcare soundscaper and runs the Making Hospitals Quiet program for Chicago Metallic Corporation. He is member of the Acoustics Working Group revising the 2010 Facility Guidelines Institute’s FGI Guidelines, and chairs the subcommittee on healthcare acoustics for the Acoustical Society of America (ASA) Technical Committee on Architectural Acoustics. Madaras can be contacted via e-mail at madarasg@chicagometallic.com.



