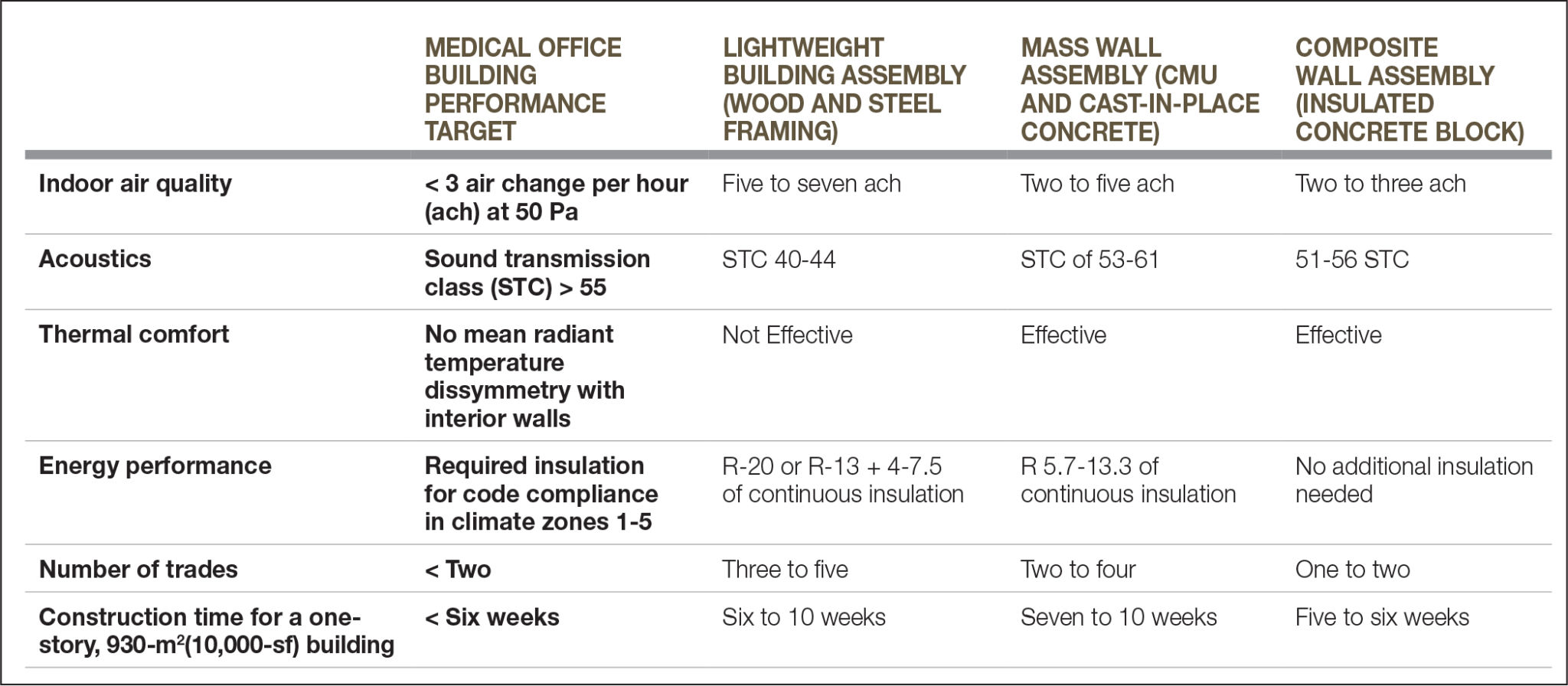
Indoor air quality
Top-tier air quality is needed for the effective care of patients in any medical office building. Providing a space that is clear of mold, mildew, volatile organic compounds (VOCs), and particulates is critical to the success of a facility. Filters included in mechanical equipment, if they are not combined with proper sealing of the building envelope, may not prevent uncontrolled air from entering a facility. A study conducted by the American Society of Heating, Refrigerating, and Air-conditioning Engineers (ASHRAE) indicates air infiltration rates in standard construction can be as many as five to seven air changes per hour (ach). This study also suggests that less than 1 ach is achievable if the wall is specified and constructed carefully. (This information comes from “Setting Air Tightness Standards,” a piece completed for the ASHRAE Journal, [vol. 47, no. 9], in September 2005.)
Thermal comfort
Patients undergoing treatment and examinations are sensitive to changes in air speed, wide bands of air temperatures, and dissimilar radiant surfaces between interior and exterior walls. In medical facilities, even modest changes in the thermal environment can create exaggerated sensations that dramatically affect patients’ mindsets and providers’ ability to support them. As such, the thermal ‘comfort zone’ for medical office buildings is generally tighter than ASHRAE 55, Thermal Environmental Conditions for Human Occupancy. A dead-band of only one to two degrees of air temperature, air speeds less than 190 cfm, and radiant temperature equal to room temperature is also suggested. (The Journal of Hygiene published R.M. Smith and A. Rae’s study, “Thermal Comfort of Patients in Hospital Ward Areas,” in 1977.)
Acoustics
Medical environments have steadily increased in volume as sirens, alarms, and urban locations have gained traction. These higher levels of background noise not only impede communication between care providers and patients, but also increase levels of stress. This can affect decision-making by care providers as well as a patient’s ability to cope and heal. To mitigate sound transmission, the enclosure should target a sound transmission class (STC) greater than 55—a number that, according to the Ceilings & Interior Systems Construction Association (CISCA), has proven to be the sweet spot needed for acoustic well-being. (The Ceilings & Interior Systems Construction Association released this information in a report, “Acoustics in Healthcare Environments” in October 2010.)
Energy performance
The effective R-value of the building envelope dictates the amount of energy required to produce and maintain performance. However, most calculations for energy performance fail to fully account for the effects of thermal bridging. Thermal bridging occurs when heat gain or loss is more quickly transferred through wood or metal studs in a lightweight building assembly (LBA), or directly through a mass wall constructed of tilt-up concrete or concrete masonry units (CMUs). To compensate for this, HVAC designers often over-size systems to ensure there is enough capacity to meet thermal comfort—a strategy which in turn leads to reliance on equipment that runs less efficiently than equipment that is properly sized.
Selecting the right enclosure system
Three categories of wall enclosures are generally used in medical office buildings:
- LBAs such as wood and steel framing;
- mass wall assemblies such as concrete masonry units (CMUs) and concrete; and
- composite wall assemblies that combine multiple materials (such as insulated concrete block).
When high air quality, acoustics, and thermal control performance standards are applied, the initial cost of wall materials is no longer the best factor to consider when determining what is best for a project. Materials that were historically hidden behind interior and exterior finishes have become the most important considerations a specifier can make. The performance of each of the wall components, and how they interact with each other, determines whether an enclosure can achieve the performance criteria listed above.
Lightweight building assemblies
Wood and steel stud cavity wall construction have historically been selected due to their low cost and easy construction. These materials are simple to find and price, and trades have been using them for years. However, once performance criteria for air, acoustics, thermal, and energy performance are considered, such LBAs rapidly become the most complex system to specify.
The challenge with lightweight framing is the number of parts to the system. Studs, sheathing, cavity insulation, continuous insulation, air/water barriers, interior finishes, and exterior finish materials all play a part in the overall performance of the system. A single poorly selected component, such as interior wallcoverings that inadvertently trap moisture in the wall, can impede the performance of the other components of the system.
Inexperienced or unskilled subcontractors can cause the same issues as badly specified components; one poorly installed material can render all the properly installed components ineffective. With the advent of field testing and envelope commissioning services to verify performance target achievement, contractors often find themselves at the center of a complex debate when test failures occur. Many parties scramble to assign fault if this happens—and must also find solutions to fix the installation after it is complete. Thus, trades that have historically functioned independently must now work together to achieve a high-performing enclosure.
Together, various medical office building performance criteria can increase the complexity of light frame construction. Speed, flexibility of parts, and the low level of skill needed for installation may all be benefits of LBAs, but all these benefits interfere with the tight, integrated, and coordinated construction necessary to fit performance criteria.